Speech - language pathologists (SLP's) are being engulfed in an identity crisis, within the community of healthcare providers. Among primary care physicians, medical speech-language pathology services are often an afterthought. Given the history of confusion over the name of its practitioners, it is confusing to their stakeholders that SLP's in healthcare now get the majority of their work from swallowing referrals. There are also concerns about the burnout rate among SLP's; the relatively flat salary schedule for healthcare clinicians; requirements by employers that their clinicians are ALWAYS available; the need to justify your existence with continually high productivity; - but there is also hope for the healthcare SLP who feels she/he is being compartmentalized as a "swallowing technician".... I actually was called that once by an internal medicine resident....mortifying, to say the least, when medical SLP's have to know how swallowing works in its complexity, and we must know how to work with people who need swallowing help. Doctors. What a mess they can make.
The medical SLP who dives into each day of swallowing problems, will swim toward an intersection of known scientific - cultural - political phenomena, that will be significantly addressed by the involvement of SLP clinicians. Sea changes in social science, in health, in politics and in culture will also serve the personal and professional growth of SLP practitioners, as we confront their effects on the field. Let's briefly identify a few of the intersecting forces, with potential to affect clinical practice patterns.

1. Dysphagia management: there is a realization that, even though the
technology exists to provide modified diets, safe to swallow by persons
with diagnosed dysphagia - the consumer may not want to eat the diet! Practice trends exist that allow the consumer and her supports
to train for swallowing a 'normal' diet, through use of compensatory
strategies. With this approach, a modified diet should be considered a
temporary intervention in the majority of dysphagia management cases. "I
can eat my favorite food, when I ____", is the outcome desired, not "I
can eat my favorite food, when it is prepared by ____". When you can offer your consumer potential to consume their preferred diet, they will often work hard for you - for THEIR goals.
2. Food viscosity: When you change the viscosity of a material, you
affect its ability to flow through a conduit. A consumer of SLP
services, who wishes to improve her swallowing of favorite foods,
will have viscosity as one powerful tool. Can you chew and manipulate a
pretzel bun to the consistency of oatmeal, through your mouth to TRIGGER
the swallow in your throat? Do you swallow the ginger ale right out of
the bottle, or does it need more mass to be easily felt and controlled
past your airway? Dedicated viscosity modifications, the product of
modern science, are easier than ever to find in pharmacies and big box
stores. Can any more natural change agents do the same? Clinical
experience says YES. Talk with your clinician for details. When you can augment the foods your consumer likes, so she can eat/drink them, they will often try their best.

3. Cooking: making not only the food easy to swallow for persons with dysphagia, but also tasty, convenient and palatable, is the mission of the family, the cooks, the servers, and the activated patient who prepares the consumer's diet. Is it served as it was intended, or is it cold? Will flavors and seasonings enhance the taste, and the enjoyment of the food and drink? Are salt, fat, acid and heat appropriately utilized to make this, the best meal your consumer has had recently? Does the place where the consumer is eating, help focusing on swallowing better? Are drinking vessels, utensils, condiments easily used? If an SLP and the consumer's supports can tailor the meal to the consumer's changing needs, then you might have the therapeutic alliance you want. The patient can eat for pleasure, while consuming an appropriately safe diet.
4. Urban farming/community gardening: giving the SLP consumer food and
drink she/he wants to eat, might include making available locally grown,
fresh and nutritionally dense food. Both urban farms and community
gardens can provide seasonal fruits and vegetables, which when grown
organically and harvested timely, can heighten the experience of eating a least restrictive diet. A consumer that enjoys easily eaten food, grown
cleanly and locally, may even want to grow some of her/his own food. When a consumer and her supports gets involved in bringing the food to their table, savoring it can make it easier to swallow.
5. Locavore: the person who eats like a locavore, regards the food grown locally and available only in season.
There may not be an immediate connection between an SLP consumer's dietary plan, and the decision to eat only locally produced food. Yet the consumer who consumes only locally grown food, helps change dependence of a food community on a global food supply chain. When you want to have a supply of a seasonal food throughout the year, you rely on traditional food preservation methods, eg canning or drying, to keep available longer, the food you want to eat. A local food consumer has a closer connection to the environments where food is grown, and where it is consumed. When you can eat seasonally, locally, cleanly, you have the best of all possible foods.
6. Culinary medicine: Approximately thirty clinical training programs
around the world help physicians learn to properly prescribe food as a
treatment for medical problems. Liaisons with nutritionists, chefs,
dieticians, food scientists, food industry representatives, consumer
groups and others may aid your family doctor, to guide you to the best
dietary solutions for your health. Will your doctor give you samples (amuse bouche) in
the office? Does the industrial food industry throw lots of money at physicians, with the goal of delivering cheap, mass marketed and convenient-to-produce food, to consumers?? When your primary care physician has access to food as medicine, you have available a medicine with centuries of proven effectiveness.
7. Food insecurity: Communities of all cultural, ethnic and economic stripes do not have adequate access to healthy food for many of its citizens. The roots of food insecurity may lie partially with limited personal income, with limited public support for food support programs and limited perspectives by the public, about the persons seeking food security assistance. Helping our food - insecure families, neighbors and communities get those resources to feed themselves, can be a rising tide that raises all boats. Food insecurity, hunger, poverty, chronic disease, economic stagnation, educational ceilings, and political instability: each are a pressure wave pushing against the stability of the culture. When food markets find their way into "insecure" neighborhoods, so that people of all levels of society have equal access to good food, we have a healthier society.

8. Environmental justice: a community resident inhales polluted air, or ingests food or drink contaminated with toxic material that endangers generations of residents. The toxic material often has an industrial source, placed in close proximity to residential areas when residents had little political power to keep the industry out. Industrial byproducts e.g. coal ash, heavy metals, and corrosive solvents accumulate in the industrial site - challenging the quality of life frmor residential sites. Industries have little incentive to clean up their byproducts, for civic leaders do not wish to alienate the generators of tax revenue and payroll for their jurisdictions. The cumulative effects of exposure to toxins for community residents, will often lead to chronic disease, if not severe afflictions that are atypical for the disease prevalence.
9. Climate change: It is a long - kindling inferno. No matter its presentation, the warming of our climates degrades our ability to grow food. Limits on water access yields limited ability to raise plants and livestock. The ecology that supports food production loses its equilibrium. Limited food production opens a Pandora's Box of stress on food and financial markets. Societies having difficulty feeding themselves will fight to control resources. When persons can't find food for themselves and their families, they will do what is necessary to survive. As data from NOAA illustrates, average annual world temperature has grown logarithmically since 1980. How much more time do we need to achieve climate justice?

10. Forest bathing: in Japan, where the practice originated, it's called 'shinrin-yoku'. A forest bather spends time in nature for refocusing, reflection and healing. Turn off and set aside your technology, when you forest bathe. You ultimately discover that the experience can be created, out of the forest. It's possible, even in your garden.
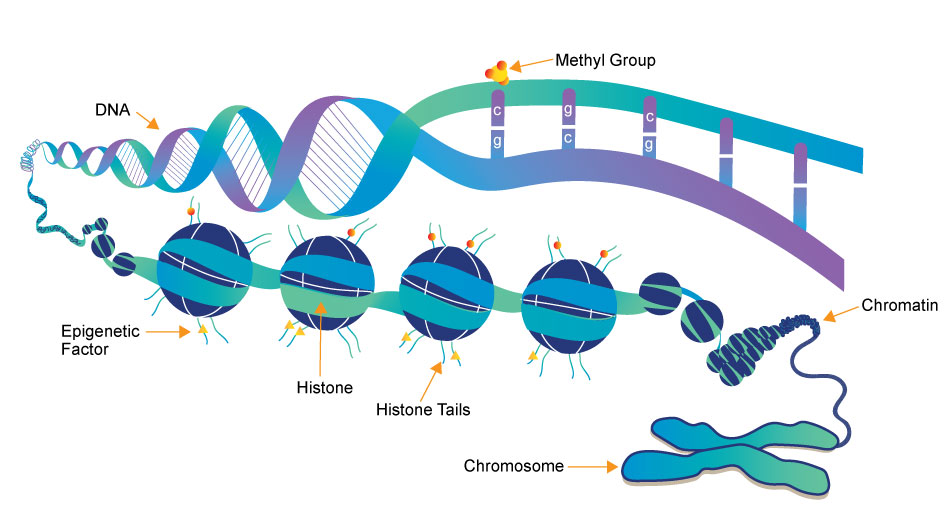
11. DoHD: The Developmental Origins of Health and Disease hypothesis suggests that critical periods, cumulative disadvantage, chains of risk and accumulation of social determinants can constitute an approach to effective management of health risk through the life span.
12. Epigenetics: social and environmental influences on health have been reflected as changes in the structure of chromosomes. Not only will your grandparents' behaviors have influenced your own health, but your health status will be reflected in the genetic potential of your descendants.
13. Life Participation Approach: in spite of significant impairments to function, including breakdowns of independent feeding and swallowing, consumers of SLP services can be helped to eat some of the foods they want. Making it possible to safely/efficiently swallow foods, might keep the consumer participating in the social network.
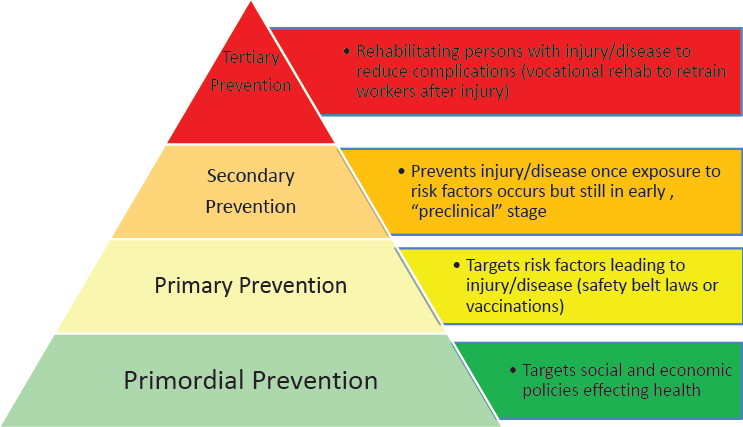
14. Primary vs. Primordial prevention: SLP clinicians who have become accustomed to prevention at the secondary level (identifying persons with impairments), will now find prevention can occur at primordial (prevention of risk factors for disease) or primary (modification of the risk factors) levels. If the SLP clinician wants to augment a clinical practice with prevention activities, e.g. assisting a consumer in improving the quality of food eaten, that clinician has a larger world in which to work. The big world will be much more conscious of what SLP does.